Approximately 13% of low back pain is attributable to the SIJ (3). Sacroiliac joint dysfunction (SIJD) can be divided into two general categories: mechanical and arthritic. “Mechanical” SIJD results from any process that alters normal joint mechanics. Common culprits include: leg length inequalities, gait abnormalities, lower extremity joint pain, pes planus, improper shoes, scoliosis, prior lumbar fusion, lumbopelvic myofascial dysfunction, repetitive strenuous activity and trauma- especially a fall onto the buttocks. Studies show that over half of mechanical SIJD results from an inciting injury (4). Pregnancy creates an array of sacroiliac joint issues with weight gain, gait changes and postural stressors occurring contemporaneously with hormone-induced ligamentous laxity. “Arthritic” SIJD results from either osteoarthritis or from an inflammatory arthropathy including; ankylosing spondylitis, psoriatic arthritis, enteropathic arthritis, and Reiter’s/reactive arthritis which produce sacroiliitis and resulting pain. Morning pain that resolves with exercise is characteristic of arthritic SIJD.
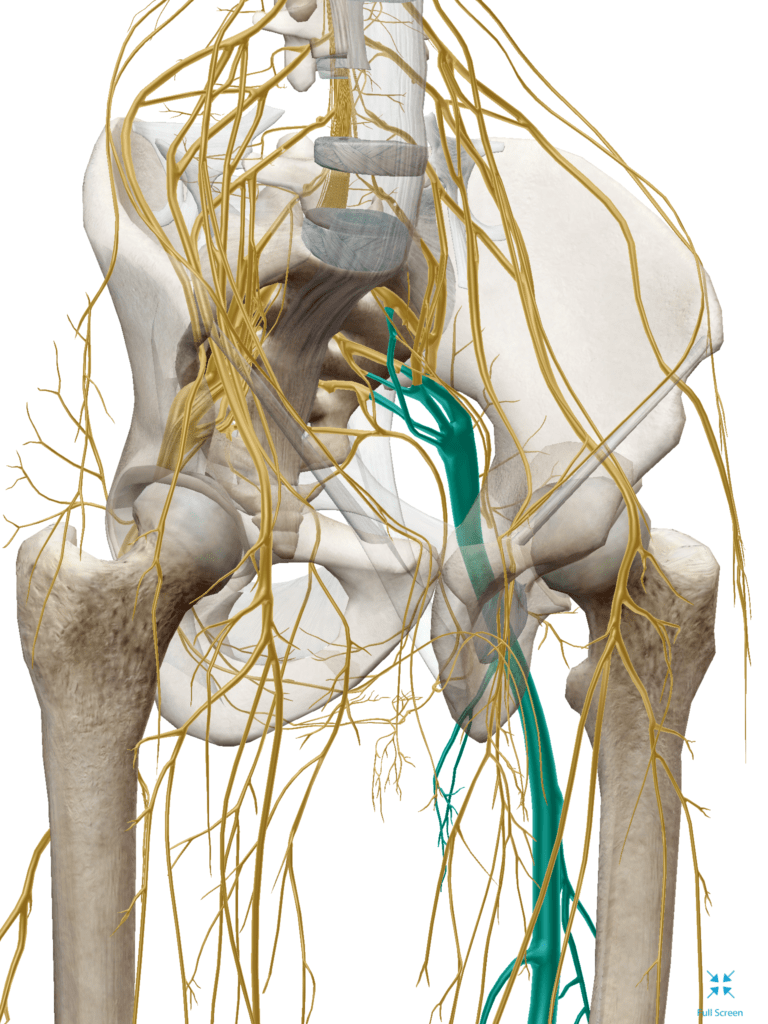
The clinical presentation of SIJD is quite variable and shares several common characteristics with other lumbar and hip problems.The patients lumbar spine must first be ruled out since it’s a common referral for low back discomfort. When asked to point specifically to the site of pain, the SIJD patient will often place their index finger over the PSIS. Pain may or may not refer to the lower back, buttock, thigh or rarely into the lower leg via chemical radiculopathy of the neighboring L5 or S1 nerve roots (5). Symptoms may be exacerbated by bearing weight on the affected side and relieved by shifting weight to the unaffected leg. Pain may be provoked by arising from a seated position, long car rides, transferring in and out of a vehicle, rolling from side to side in bed or by flexing forward while standing. Pain is often worse while standing or walking and relieved by lying down.
References
1. Sturesson B, Selvik G, Uden A. Movements of the sacroiliac joints: A roentgnen stereophotogrammetric analysis. Spine. 1989;14:162–165.
2. Sturesson B, Uden A, Vleeming A. A radiostereometric analysis of the movements of the sacroiliac joints in the reciprocal straddle position. Spine. 2000;25:214–217.
3. Maigne JY, Aivaliklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation tests in 54 patients with low back pain. Spine 1996;21: 1889–1892.
4. Bernard TN Jr, Kirkaldy-Willis WH. Recognizing specific characteristics of nonspecific low back pain. Clin Orthop Relat Res. Apr 1987;217:266-80.
5. Fortin JD, Washington WJ, Falco FJE. Three pathways between the sacro-iliac joint and neural structures. AJNR. 1999;20:1429–1434.