Jaw Pain
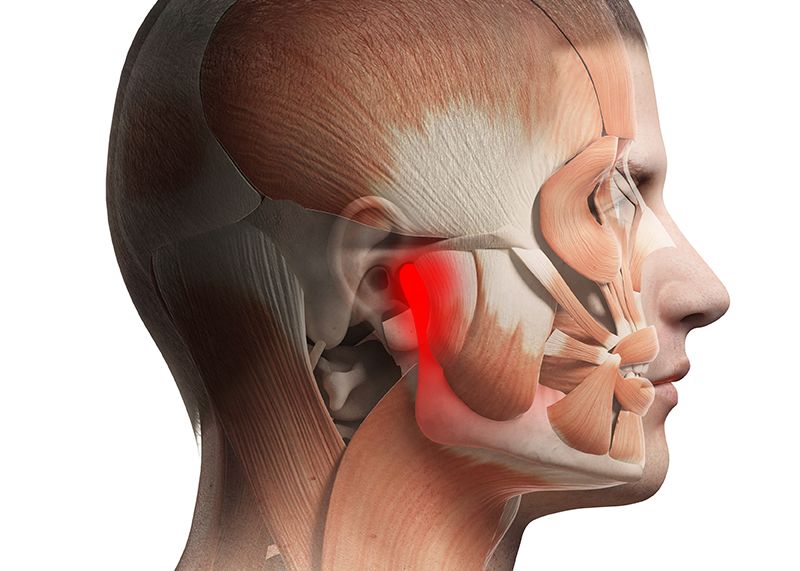
The temporomandibular joint otherwise known as the “jaw” can be a very frustrating area of pain for individuals and can be very debilitating due to the nature of the symptoms and location of the joint on the face. What most individuals don’t know is that jaw pain can often very closely tied to the neck and upper extremity due to proximity and via the nerves that innervate the jaw. The joint itself is the articulation of the mandibular condyle on both sides connecting with the temporal bones with two discs in between, which is why individuals can often experience headaches in conjunction with jaw pain. The temporomandibular joint has 5 motions depression (mouth opening), elevation (mouth closing), protrusion (Chin forward), retraction (sliding teeth backwards) and lateral deviation.
When the jaw or related don’t move as they’re supposed to you can often times experience headaches, facial pain, neck discomfort or pain with eating. Due to the proximity of the TMJ to the ear, an individual may also experience ear-related symptoms such as an earache or tinnitus. Some of the signs that you may have temporomandibular joint dysfunction include facial, head or neck trauma, asymptomatic clicking and potentially even orthodontics early in life.
The most commonly assessed motion associated with TMJ dysfunction is Mandibular depression or “opening the mouth”. The normal opening distance of the mouth should be 3 knuckles, but there is individual variation in this measurement. One of the dysfunctional movement patterns associated with opening the mouth could include a “C curve” in which the jaw deviates to the dysfunctional side before “clunking” into position at the end of opening.
Because the jaw is so intimately connected with the cervical spine (neck), individuals will often describe symptoms that change with cervical movements of the neck. For example, a common motion that is associated with TMJ discomfort is cervical flexion or looking downwards. This is why at our office, after we have taken a thorough history and assessed all movements of the jaw and neck, we will begin our repeated motion exam with the cervical spine. If a repeated motion of the cervical spine can change the intensity, frequency or location of the jaw pain, we know that there is a cervical component to the condition and we must explore it further. If movement of the neck do not change the symptoms, we will proceed to assess repeated motions of the temporomandibular joint itself to find the position of relief.
The action of breathing can also be intimately related to jaw pain. Breathing is meant to be a very passive process in which air fills the lungs and pushes the diaphragm down symmetrically, creating pressure in the abdomen and then expanding the ribs and sternum. Many individuals use large muscle groups such as the trapezius to lift their chest excessively and breathing air into only their upper lung fields. Not only can this biomechanically put undue stress on the cervical spine and TMJ, but this also decreases mobility in the thoracic spine and inhibits the parasympathetic nervous system (rest and digest). Being in a state of sympathetic tone and high muscle tension can put a tremendous amount of stress on the jaw and muscles of the face, results in pain and poor mobility.
The last component to assessing and treating the temporomandibular joint is mobilizing the joints and muscles around the jaw. There are numerous muscles that act on and around the jaw itself such as the masseter, temporalis, trapezius, levator scapula, scalenes, digastrics and pterygoids that all can hold excessive tension leading to undue stress on the jaw. In addition, all of the joints of the cervical and upper thoracic spine can become blocked and lead to improper motion and excessive tightness throughout the neck, face and jaw. By inhibiting these muscles and mobilizing these joints, we can be sure that you temporomandibular joint is in a position to heal and regain full function and motion, pain free.